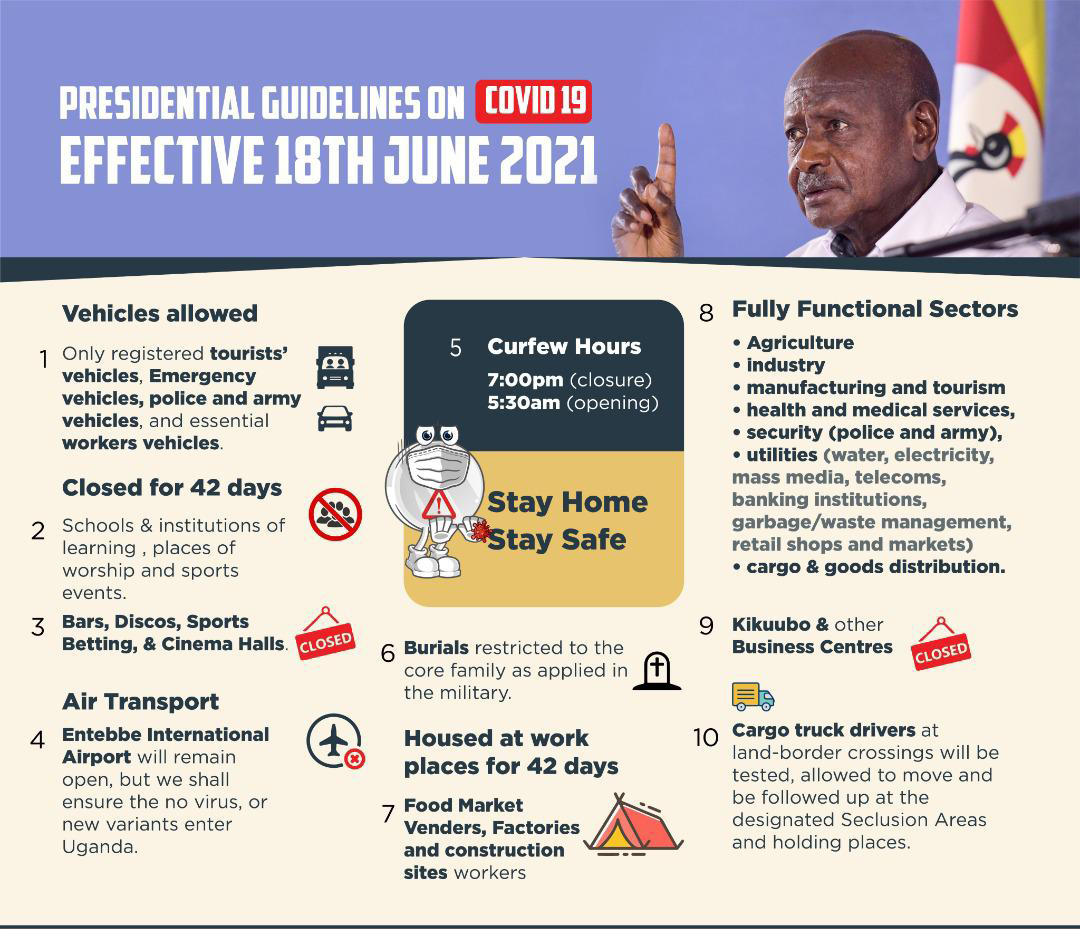
The COVID-19 situation in Uganda has worsened significantly in the past month as the country faces a dramatic rise in COVID-19 cases and lack of access to vaccines. Over the past several weeks, case counts have risen from just a few hundred per day to more than 1,500 per day. The Ministry of Health (MoH) has confirmed a total of 71,543 cases and 660 deaths. The actual numbers are believed to be much higher as there are only a few thousand samples tested daily. Community spread is high and testing currently shows a nearly 20% positivity rate. The government imposed a lockdown on June 7 which limited movement across the country, closed some non-essential businesses and schools, and ordered a curfew.
Less than two weeks later – on June 18 – the government announced a much stricter lockdown given the continued exponential growth of cases across the country. This included a total ban on transport between districts and all means of public transportation. Only essential workers are permitted to move around to do their work – thankfully, palliative care teams are able to continue their essential work. This current lockdown is set to last for six weeks, though that could be extended depending on how the situation evolves.
PCAU continues to play a key role on national COVID-19 committees, particularly in the areas of psychosocial support and mental health as well as case management. They are also supporting hospices as those organizations continue to provide care to their patients during these difficult circumstances. At the time of the initial lockdown on June 7, PCAU immediately mobilized to get the Road to Hope children back home safely. They are now working to support the children who are once again at home. Tutoring is not possible given the terms of the lockdown, nor would it be completely safe, so PCAU is working on the best ways to keep in touch with the children over the phone and have supplies sent to them at home. As essential workers, the PCAU team continues to conduct work in person when necessary and virtually where possible.

UNICEF and WHO officials receiving the initial batch of COVID-19 vaccines at Entebbe International Airport in Uganda.
Credit: WHO/Uganda
COVID-19 vaccination is underway in Uganda through COVAX, a global collaborative platform to support COVID-19 vaccine development and equitable access across the globe. The first shipment of vaccines that arrived in March contained 964,000 doses and another 2.7 million were expected in June from India, but these were held back given India’s own COVID-19 surge. France just donated more vaccines to COVAX, with 175,000 of them allocated for Uganda. Uganda has had difficulty in accessing an adequate supply of vaccines for its 45 million people. So far, only about 1.8% of Uganda’s population has been vaccinated with the first dose of the AstraZeneca vaccine – less than 1% have been fully vaccinated. Health care workers were prioritized in the first group to be vaccinated, though many had only received their first dose when this wave hit the country.
Despite the strict lockdown, Uganda’s health system is burdened by increasing severe infections. In announcing the second lockdown, the president said that hospitals are full. According to the MoH, they are seeing a sharp increase in cases among younger people, with those between 20 and 39 years being hit the hardest. Health care workers are reporting shortages of essential supplies including oxygen. The government is trying to move quickly on the installation of a new oxygen plant at Mulago, the national referral hospital, but more will need to be done for patients in rural areas. The Minister of Health has stated that the greatest challenge is human resources – health care workers are already in short supply in Uganda, and just as health care workers around the globe, they are fatigued from this pandemic.

A cohort of nurses from the Advanced Diploma in Palliative Care Nursing program at Mulago School of Nursing and Midwifery. The CHC/HF and PCAU Partnership has supported this effort to help increase the number of trained palliative care workers throughout Uganda. Note: this photo was taken before the COVID-19 pandemic.
The COVID-19 situation is worsening across many countries in Africa. In early June, the World Health Organization (WHO) regional director for Africa, Dr. Matshidiso Moeti, said, “The threat of a third wave in Africa is real and rising. Our priority is clear – it’s crucial that we swiftly get vaccines into the arms of Africans at high risk of falling seriously ill and dying of COVID-19. While many countries outside Africa have now vaccinated their high-priority groups and are able to even consider vaccinating their children, African countries are unable to even follow up with second doses for high-risk groups.”
The WHO believes we have a very short window of time to utilize the vaccines we have to combat the current variants, which remain largely susceptible to these vaccines. This includes the Delta variant which is more dangerous to those vulnerable to the disease. Experts believe this variant, along with five others identified in the country, are driving the surge in cases in Uganda. The MoH is emphasizing that complacency has been a problem as well. Vaccines must be combined with crucial public health measures to bring this wave under control and reduce the spread of COVID-19.
For the most recent statistics on the COVID-19 situation on Uganda, please visit the Government of Uganda, Ministry of Health’s website.
For a look at other countries or the continent as a whole, please visit the Africa CDC website.